Designing glaucoma care pathways using GLAUC-STRAT-FAST
The College of Optometrists and The Royal College of Ophthalmologists have developed the following guidance in response to the National Institute for Health and Care Excellence (NICE) NG81 Glaucoma: diagnosis and management guidance to enable high-quality care for glaucoma patients, using the wide range of professional skills available.
The Colleges’ joint guidance aims to empower optometrists and other healthcare professionals (HCPs) in primary and secondary eye care to contribute to glaucoma care. This will increase capacity, reduce the backlogs which put patients at risk of permanent and avoidable sight loss, and improve patient experience.
The guidance maps optometrists’ qualifications and training to the different categories of glaucoma risk, as set out by the GLAUC-STRAT-FAST risk tool. The guidance highlights the need for glaucoma care pathways to fully recognise and utilise local optometrists’ competences, and specifies which qualifications are required for autonomously managing patients in different risk categories.
The guidelines specify that services should be configured to meet patient demand, and developed using robust risk stratification.
Introduction
Ongoing glaucoma care is delivered in a wide range of environments, by several professional groups and with differing levels of training, accreditation, experience, and supervision provided by consultant ophthalmologists. Multiple models of care have evolved across the NHS. They range from classical consultant-led face to face outpatient clinics in hospital utilising a multidisciplinary team to ‘virtual clinics’ with decision making remotely based on diagnostic data to ‘shared-care’ or ‘co-management’ with primary care optometrists. It is crucial that we empower the whole multidisciplinary ophthalmic team in primary and secondary care to safely contribute to glaucoma care, to increase capacity and thereby reduce the backlogs which put patients at risk of permanent and avoidable sight loss and improve the patient experience. This needs to be done based on robust risk stratification.
The UKEGS/RCOphth GLAUC-STRAT-FAST tool provides guidance on how patients with glaucoma-related conditions can be risk stratified based on their lifetime risk of developing visual loss.
| GLAUC-STRAT-FAST | ||
| R1 Advanced 1° Open Angle / Angle-Closure Glaucoma | R2 Developmental Glaucoma | R3 Surgical Glaucoma (peri-operative) Progressive Glaucoma (reliable VF changes) |
A1 Early 1° Angle-Closure Glaucoma (<4dB) Early 2° Glaucoma (<4dB) | A2 Moderate 1° Angle-Closure Glaucoma | A3 Moderate 2° Glaucoma |
G1 Glaucoma Suspect | G2 1° Angle-Closure | G3 1° Angle-Closure Early 1° Open Angle Glaucoma |
| >8 dB | Red Flag (Consider as RED)
| |
| 4-8 dB | Plus (+) Factors (More complex) Ophthalmic co-morbidity
Systemic / social factors
| |
<4 dB If loss <5° from fixation or Angle-closure / 2° Glaucoma | ||
| <4 dB |
The aim of this supplementary guidance is to summarise existing guidelines to show how currently available training and qualifications enable Health Care Professionals (HCPs) to deliver care for patients with different categories of GLAUC-STRAT-FAST risk. Current guidelines and qualifications relate specifically only to some of these risk categories. The design of care pathways will need to consider the competences available in the local workforce and the degree of consultant / hospital ophthalmic team supervision, and interpretation of the recommendations within a local clinical governance framework with multidisciplinary clinical professional leadership. This will enable the delivery of high-quality care using the wide range of professional skills available, in current and innovative service models.
2 Current guidelines, qualifications, and competencies
The NICE Glaucoma: Diagnosis and Management NG81 Guidelines (2017; 2022) and the previous NICE CG85 (2009) set the core direction for glaucoma service design, broadly specifying the levels of patient risk and the skills set necessary to diagnose, monitor and manage glaucoma and related conditions. The RCOphth Commissioning Guide: Glaucoma (2016) maps this information against the higher professional qualifications available to HCPs to indicate the levels of skills required to deliver care in various scenarios. However, since these were published numerous new models of care have emerged, the new risk stratification tool has provided more clarity on risk levels, and there are more in-hospital qualifications available.
2.1 Optometric core competence
Some patients at very low risk of developing glaucoma (a proportion of patients in G1 – see below Table 1) who do not require monitoring, can be discharged to regular sight tests. NICE NG81 (2022) states:
- Advise people with IOP below 24 mmHg to continue regular visits to their primary eye care professional. [2017] (NICE NG81 1.1.7)
- Do not offer treatment to people with suspected COAG and IOP less than 24 mmHg unless they are at risk of visual impairment within their lifetime. Advise people to continue regular visits to their primary eye care professional, at clinically appropriate intervals. [2017, amended 2022] (NICE NG81 1.4.11)
- Discharge people back to primary eye care services if:
- they were referred for OHT but do not need treatment
- they were referred for suspected COAG but this is no longer suspected
- Advise people that they should continue with regular visits to their primary eye care professional, at clinically appropriate intervals. [2017] (NICE NG81 1.5.14).
2.2 The College of Optometrists Levels of higher qualifications for health care professionals
The College of Optometrists offers a series of higher qualifications for optometrists and other HCPs to advance their skill set above those of core competency. The courses and their assessments are delivered by academic partners prior to the awarding of the qualification by the College of Optometrists. It is useful to note that the Higher Certificate and Diploma require the optometrist or HCP to undergo extensive further clinical training in a secondary care setting with a specified number of glaucoma patients seen and involve skills development through clinical placements.
The higher qualifications provide an ascending three-level order of skills development:
The Professional Certificate in Glaucoma is designed to prepare practitioners to participate in formal enhanced case finding programmes and OHT/ suspect COAG monitoring schemes.
The Professional Higher Certificate in Glaucoma is designed to prepare practitioners for participation in primary care or hospital-based schemes involving the diagnosis of OHT and preliminary diagnosis of COAG. It includes assessment in competence in gonioscopy, and further develops practitioners’ ability to detect change in clinical status, subsequent decision-making, as well as management of patients with OHT and usually also suspect glaucoma.
The Professional Diploma in Glaucoma aims to prepare practitioners to provide either a primary care glaucoma service, or to work with a high degree of autonomy within a hospital glaucoma clinic, making appropriate evidence-based management decisions.
The Independent Prescribing (IP) qualification: NICE guidelines NG81 clearly indicate that an IP qualification alone is insufficient for glaucoma practice. However, when combined with the Higher Certificate or Diploma in Glaucoma, the IP qualification enables the autonomous therapeutic management of cases according to the appropriate risk stratification, under the local governance arrangements for NHS funded care.
2.3 Ophthalmic Practitioner Training (OPT)
The OPT has been designed as training for the non-medical workforce within a secondary care setting in a structured, standardised and transferrable way. The curriculum covers the 4 highest volume areas in ophthalmology: Cataract, Glaucoma, Medical Retina and Emergency Ophthalmology. It is based on the existing framework for ophthalmology trainees and introduces a medical model of training to HCPs working in secondary care. The OPT curriculum defines a minimum standard of competence and encourages learners to develop skills beyond this minimum.
It is a competency-based curriculum, and therefore requires that, rather than just having knowledge and skill, the practitioner is assessed on their performance in the workplace through Workplace Based Assessments (WBAs) and other evidence collected and presented in a portfolio. Each subspecialty area above is separated into 3 levels:
Level 1 – Ophthalmic Clinical Practitioner
- Perform clinical work to assist medical decision making
- Participate in triage/screening
- Monitor low risk patients with an established diagnosis to a clearly defined protocol
Level 2 – Ophthalmic Specialist Practitioner
- Work to protocol with clearly defined delegated decision making
- Make preliminary diagnosis within a specific area
- Manage under specific protocols
Level 3 – Ophthalmic Advanced Practitioner
- Make decisions independently with appropriate support and back up
- Diagnose, manage, and discharge within specific areas
- Role in service development and teaching
The OPT is designed primarily to support and develop HCPs working within a managed secondary care environment, implying some degree of consultant supervision.
3 Linking risk and professional expertise
The GLAUC-STRAT-FAST guidance provides greater clarity on individual clinical risk and supports integrated service design proportionate to that risk. It provides more context for utilising OPT and the College of Optometrists’ Glaucoma qualified practitioners to see the right patient at the right time. The principle is that the higher the risk, the more senior the level of clinical professional involvement or supervision. Plus (+) factors should be considered a potential indicator for care at a higher level. The presence of specific red flags or the transition of an individual patient to a higher risk level identifies the need for consultant /senior decision maker involvement.
On this page, we have indicated the levels of qualification and supervision that are required for patients with glaucoma in different risk categories. It is crucial to remember that in glaucoma the level of risk for any individual patient may change with time, both up and down.
3.1 Qualifications for independent / autonomous HCP practice
The GLAUC-STRAT-FAST risk levels and equivalent proposed levels of qualification required to manage these patients are mapped in Table 1. They cover a range of risk from G1 to A3 (and possibly even R1). Whilst autonomous practice is appropriate in these circumstances, all HCP glaucoma care needs to be undertaken within an overarching whole pathway governance structure for NHS funded care. No matter where the care is delivered, pathways require supervising consultant ophthalmologist involvement within joint clinical leadership (medical and non-medical). However, as the individual HCPs are working autonomously under their own professional qualifications and within their scope of competence, the supervising consultant is not responsible for their individual performance or actions which are governed by the appropriate regulator (e.g. NMC, GOC) but should support them in their practice, development and pathway governance. It is important that any pathway commissioned is integrated so that patients whose risk status alters can move seamlessly between different aspects of the care pathway without any further referral management.
The qualifications for patients with angle-closure needs specific consideration. RCOphth ‘Management of angle -closure glaucoma’ guidance (in draft to be published shortly) covers the detection and management of angle closure and suspect angle closure. It states that ‘gonioscopy remains the definitive examination for diagnosis and monitoring angle-closure disease’. It advises that patients with angle-closure should only be referred if they fit the NICE referral criteria of raised intraocular pressure or suspect glaucomatous damage. In addition, patients with PACS PLUS require referral. PACS minus patients can be monitored by optometrists with core competence where commissioned and receive regular eye examinations.
Table 1: Scope of autonomous practice for HCPs with further qualifications
| R1 Diploma in Glaucoma$ OPT Level 3$ | R2 Diploma in Glaucoma OPT Level 3 (depending on case complexity) | R3 |
| A1 Diploma in Glaucoma OPT Level 3 | A2 Diploma in Glaucoma OPT Level 3 | A3 Diploma in Glaucoma OPT Level 3 |
| G1 Professional Certificate in Glaucoma£ OPT Level 3 | G2 Higher Certificate in Glaucoma* OPT Level 3* (except PACS MINUS patients – core competence) | G3 Higher Certificate in Glaucoma* and OPT Level 3* - 2o OHT, 1o Angle Closure Diploma - Early 1o OAG |
*Whilst Primary Angle Closure is not noted specifically in training outcomes these qualifications include skills in gonioscopy and are hence deemed essential to manage patients with these conditions.
($) There is no specific definition of ‘advanced’ in the curriculum for the Diploma in Glaucoma or OPT Level 3. Involvement of health professionals qualified to this level on the management of R1 patients will depend on local training and governance processes.
(£) Higher Certificate for managing, Professional Certificate for monitoring not managing.
Table 2: Clinical assessment, when adequately supervised via virtual review of each patient by reviewer with qualifications according to Table 1, in primary care or secondary care settings.
| R1 Core competent optometrist or HCP | R2 Core competent optometrist or HCP | R3 Core competent optometrist or HCP |
| A1 Core competent optometrist or HCP | A2 Core competent optometrist or HCP | A3 Core competent optometrist or HCP |
| G1 Core competent optometrist or HCP | G2 Core competent optometrist or HCP | G3 Core competent optometrist or HCP |
(Exception: any primary or secondary angle closure condition, except PACS minus, which require gonioscopy – Higher Certificate or OPT level 3)
3.2 Qualifications for HCP for virtual clinics
Patients within GLAUC-STRAT-FAST categories G1 to G3 and A1 to A3 are potentially suitable to be monitored using attendances in which clinical data is captured and later reviewed virtually by a clinical decision-maker, so called virtual clinics. The clinical decision-maker may be an optometrist, other HCP or ophthalmologist in primary or secondary care, with appropriate qualification. There is already considerable provision of care in this way, and it is rapidly expanding. Patient assessment may take place in a variety of locations - primary care, community diagnostic hubs or hospitals and is often undertaken by technicians. Such virtual pathways require the same clinical governance framework as face-to-face care – decisions on patient care are made by those with the appropriate competences, consultant advice and supervision are available, with outcomes and patient experience audited.
In a virtual pathway, where an HCP is the autonomous decision maker reviewing the data and making the decisions on all aspects of care, the requirements for qualifications against the risk of the patient are as in the above section on autonomous practice and summarised in Table 1.
However, there are a range of models of virtual pathways involving HCPs which include HCPs sharing data and findings without contributing a clinical decision or management plan (for which, in primary care optometry, core competency is sufficient) and blended models where there is a degree of decision making by the HCP but with more virtual support or consultant “supervision” than an autonomous decision maker. There is currently no formal definition of consultant supervision in this context.
Responsibility lies with local clinical governance processes for ensuring that HCPs have the appropriate level of clinical competence and decision-making ability, whatever the model of care, for any given patient risk level.
However, it is crucial to ensure the following principles are met:
- The clinician who reviews the results needs to possess the appropriate competence for the risk level of the patients being reviewed and the understanding of when to seek advice or transfer patients to face-to-face clinics
- Except when the final responsibility for a patient rests with an appropriately qualified HCP, such as an optometrist with the diploma in glaucoma, the governance of a pathway must involve the consultant ultimately responsible for a patient. This is irrespective of whether the pathway crosses locations, professions, or provider organisations
- HCPs involved in data collection and preliminary patient assessment are able to obtain senior medical or consultant advice, in addition to the normal process of ‘virtual’ consultant patient review eg for urgent issues.
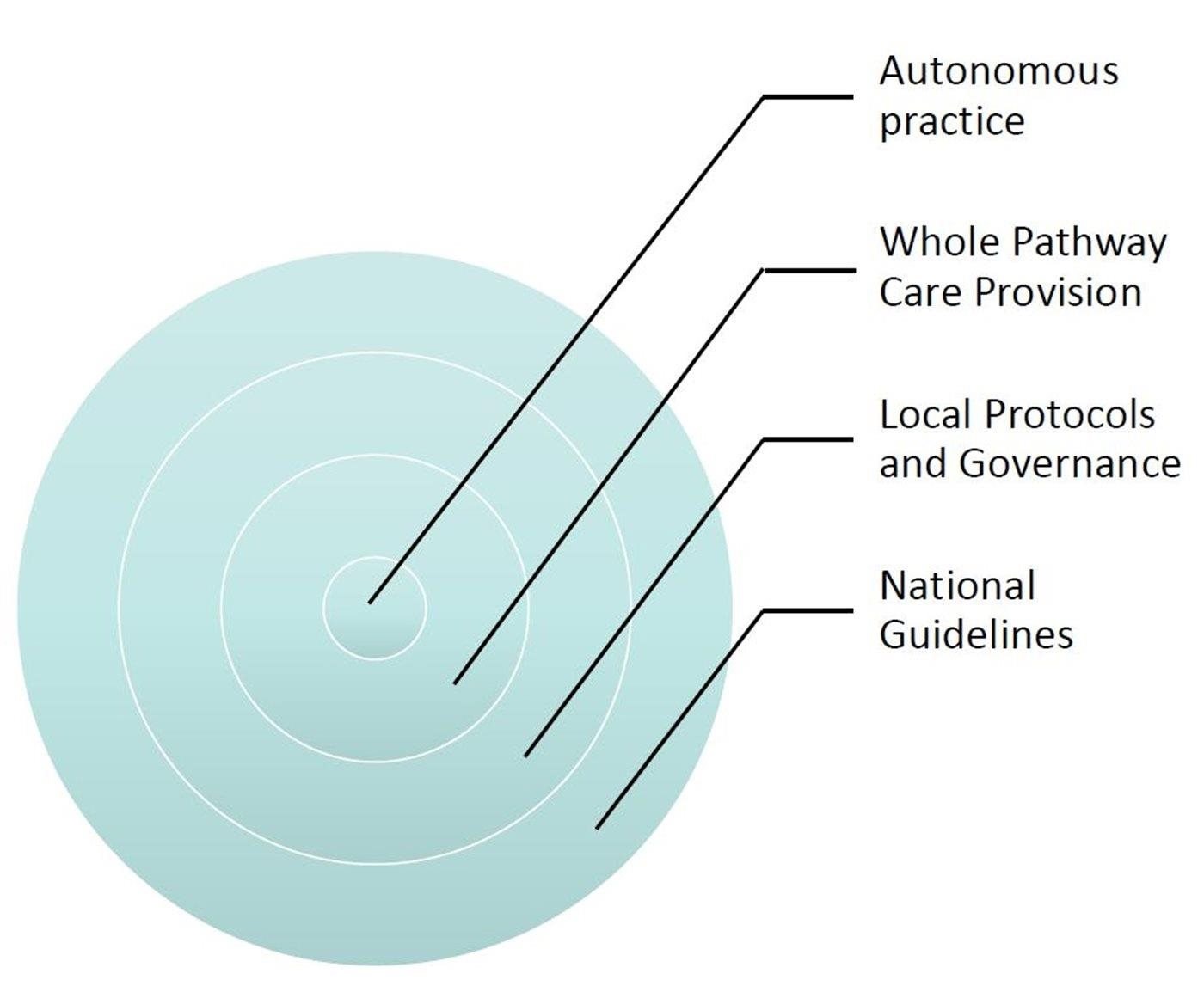
Figure 1 – Autonomous practice sits within a whole glaucoma pathway which is controlled by local protocols and governance which in turn is informed by national guidelines.
3.3 Qualifications for HCP in consultant-led face to face clinics
Patients in GLAUC-STRAT-FAST categories R1 to R3 and those showing a red flag should be seen in consultant-led face-to-face clinics where the consultant is present and directly overseeing care. These clinics may be delivered by a range of professionals but their complexity and risk level is such that the physical availability of a consultant to monitor their condition and discuss treatment options is necessary. According to NICE NG81, HCPs working under supervision should possess (understood to include HCPs training for), the same qualifications for given complexity and risk level as for autonomous practice. High risk glaucoma patients represent a relatively small proportion of individuals in the glaucoma patient population, but they often require frequent visits. Clinic list size to assess these categories of patients should be adjusted to reflect the complexity (and therefore longer timing) of the consultation.
A wider range of other patients, beyond R1-3, may also be seen by HCPs in consultant led clinics in primary or secondary care where the consultant supervises and closely oversees decisions but may not always be physically present in the clinic.
As with virtual clinics, the model of HCP care in hospital varies from using HCPs as purely data collectors with all their cases reviewed to validate their preliminary decision making, to protocol driven decision making within a framework of clinical governance, audit, and systematic quality control, or working directly alongside the consultant and discussing cases when necessary. These approaches require some flexibility to ensure clinic capacity and practitioner skill use is optimised. For example, the involvement of Higher Certificate trained optometrists or other HCPs in care for A1-A3 and R1-R3 could be seen as falling outside of the letter of NICE NG81 guidelines. However, their role in supervised practice needs to be taken in the context of their skills, further training towards the Diploma and the degree of supervision. The care for all patients whose condition falls outside the autonomous competencies of the examining practitioner should be the responsibility of a suitably qualified supervising clinician and risk assessed, considering the factors above. In the case of consultant led face to face clinics in secondary care, the final decisions as to the involvement of staff in care provision will depend on a supervising consultant’s discretion based on observed skills, experience, and levels of direct supervision.
4 References
1. The Royal College of Ophthalmologists, Clinical Council for Eye Health Commissioning. Commissioning Guide: Glaucoma (2016), June 2016
2. The College of Optometrists. Higher Qualifications in Glaucoma
3. Health Education England, The Ophthalmic Common Clinical Competency Framework – Curriculum.
4. National Institute for Health and Care Excellence. Glaucoma: diagnosis and management, NICE Guideline [NG81], November 2017
5. National Institute for Health and Care Excellence. Glaucoma: diagnosis and management, NICE Guideline [NG81], updated 26 January 2022.
5 Authors

Mr Wojciech Karwatowski

Consultant Ophthalmologist and RCOphth

Miss Angela Whitaker BSc MCOptom DipTp(IP) DipOC DipTp(AS) DipTp(SP) DipGlauc Prof Cert Med Ret

Optometrist and The College of Optometrists
The authors would like to thank the members of the UK and Eire Glaucoma Society for their help and input in the drafting of this document.
Appendix - practical summary
| GLAUC-STRAT-FAST | |||
| Risk level | R1 Advanced 1° Open Angle | R2 Developmental Glaucoma | R3 Surgical Glaucoma |
| Autonomous practice | Diploma in$ Glaucoma OPT Level 3$ | Consultant Diploma/OPT Level 3 (Depending on case complexity) | Consultant |
| Under supervision or virtual review% | Core competent optometrist or HCP | Core competent optometrist or HCP | Core competent optometrist or HCP |
| Risk level | A1 Early 1° Angle-Closure Glaucoma (<4dB) Early 2° Glaucoma (<4dB) | A2 Moderate 1° Angle-Closure Glaucoma | A3 Moderate 2° Glaucoma |
| Autonomous practice or reviewer grade | Diploma in Glaucoma OPT level 3 | Diploma in Glaucoma OPT level 3 | Diploma in Glaucoma OPT level 3 |
| Under supervision or virtual review% | Core competent optometrist or HCP | Core competent optometrist or HCP | Core competent optometrist or HCP |
| Risk level | G1 Glaucoma Suspect | G2 1° Angle-Closure | G3 1° Angle-Closure Early 1° Open Angle Glaucoma |
| Autonomous practice or reviewer grade | Professional Certificate in Glaucoma£ OPT Level 3 | Higher Certificate in Glaucoma* OPT Level 3* (except PACS MINUS patients – core competence) | Higher Certificate in Glaucoma* and OPT Level 3* - 2° OHT, 1° Angle-Closure Diploma Early 1° OAG |
| Under supervision or virtual review% | Core competent optometrist or HCP | Core competent optometrist or HCP | Core competent optometrist or HCP |
| >8dB | Red Flag (Consider as RED)
| |
| 4-8 dB | Plus (+) Factors Ophthalmic Co-morbidity
Systemic/ Social Factors
| |
| <4 dB If less <5º from fixation or Angle-Closure/ 2º Glaucoma | ||
| <4 dB |
(*)Whilst Primary Angle Closure is not noted specifically in training outcomes these qualifications include skills in gonioscopy and are hence deemed essential to manage patients with these conditions.
($) There is no specific definition of ‘advanced’ in the curriculum for the Diploma in Glaucoma or OPT Level 3. Involvement of health professionals qualified to this level on the management of R1 patients will depend on local training and governance processes.
(£) Higher Certificate for managing, Professional Certificate for monitoring not managing.
(%) Exception: any primary or secondary angle closure condition, except PACS minus, which require gonioscopy – Higher Certificate or OPT level 3.
Download
Jointly written by: